Study: Appalachian Kentuckians continue to face higher colorectal cancer mortality rates
Researchers at the University of Kentucky have found that for much of the past two decades Appalachian Kentuckians have been more likely to die from colorectal cancer compared to the rest of state and country’s population.
The study “Colorectal cancer-related mortality trends in Appalachian Kentucky from 1999-2020: A persistent healthcare disparity” was recently published in the journal Gastroenterology.
The study used data from the Centers for Disease Control and Prevention’s WONDER database to identify and analyze trends in mortality related to colorectal cancer — which, according to the American Cancer Society, is the second most common cause of cancer deaths. The patients included in the study were all aged 15 or older.
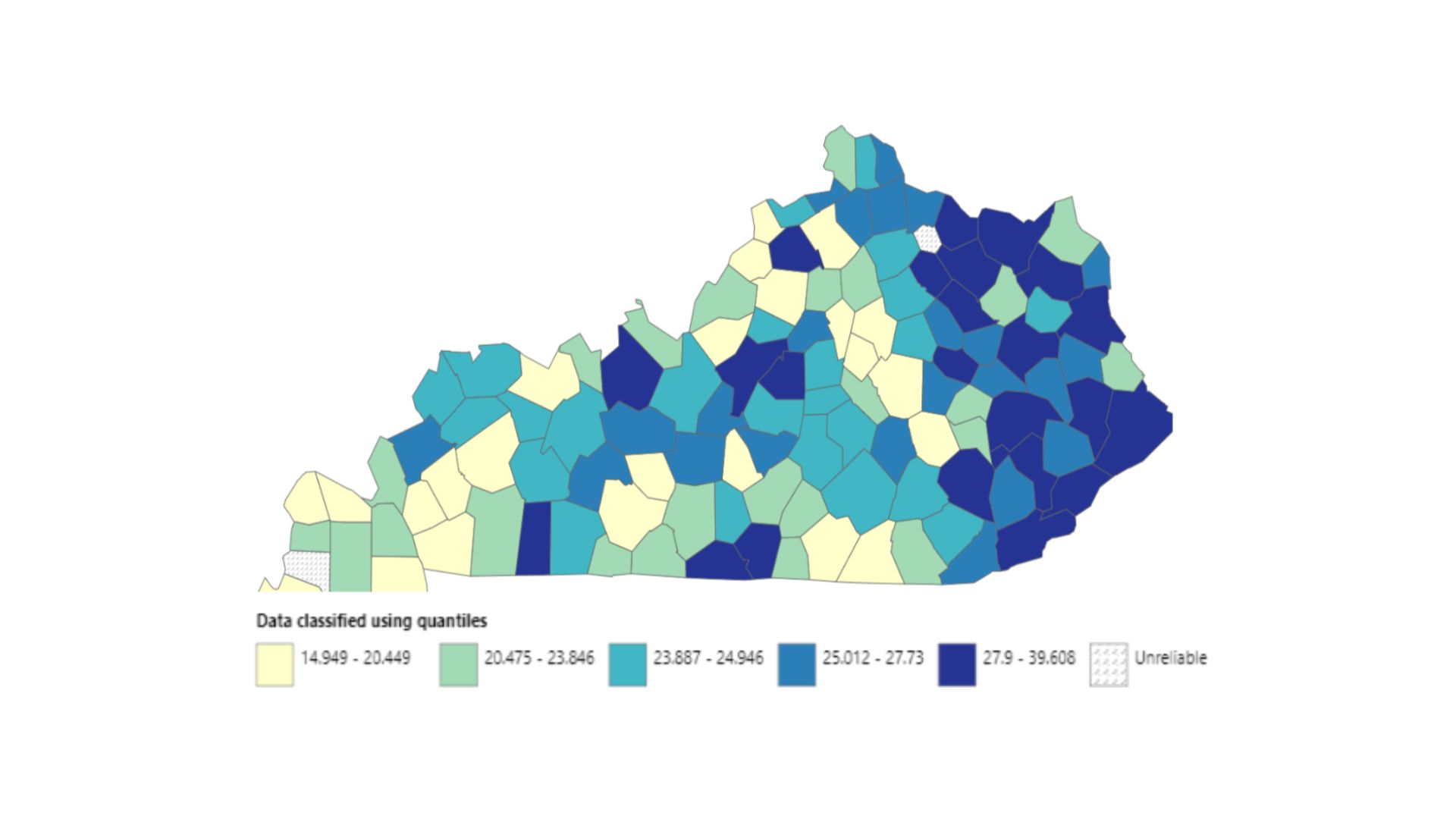
From 1999 to 2020, nearly 26 of every 100,000 people in Kentucky’s Appalachian counties died on average annually from colorectal cancer. In the state’s non-Appalachian counties that number was closer to 22. Nationwide, the annual mortality rate was 19.43 deaths per 100,000 people.
“We are definitely at risk of this becoming a persistent national health care burden which will negatively influence the health of generations to come,” said Syed Hassan, M.D., a research coordinator/clinical research scientist within the Department of Internal Medicine and lead author of the study.
Over the 21-year period examined by the study, colorectal cancer deaths across the U.S. dropped from 27 people in every 100,000 in 1999 to 14.81 in 2020.
Kentucky, however, hasn’t seen quite as steep of a drop. The persistence of deaths from the disease is more pronounced in Kentucky’s 54 Appalachian counties, as defined by the Appalachian Regional Commission. In 1999, that region saw 31.24 deaths per 100,000 people which then dropped to 24.46 in 2020.
Financial, educational and accessibility barriers in the region could be leading to the higher rate of colorectal cancer deaths, said Hassan.
In Appalachian Kentucky, nearly 41% of the colorectal cancer deaths occurred at the decedent’s home, suggesting that access may have been an issue especially for patients who might be disabled or aren’t seen by a doctor until the cancer has significantly advanced.
“That’s concerning, in my opinion,” Hassan said. “Access to health care, lifestyle related modifiable risk factors and education are important factors we should further work upon.”
In addition to access, anxiety about getting screened for the cancer and a lack of education about the disease might have also played a role, Hassan said, and those various barriers warrant further study.
“Many of these patients might’ve believed that they probably wouldn’t be able to afford as much care due to their socioeconomic status,” said Hassan, who also recently presented the study’s findings at Digestive Disease Week in Washington, D.C.
This study builds on the work of Terrence A. Barrett, M.D., the Marcos Lin Andrade Endowed Chair and professor in the Department of Internal Medicine in the UK College of Medicine, and Courtney Perry, D.O., an assistant professor in the Department of Internal Medicine. The two previously found higher health care use in patients in Appalachia with inflammatory bowel disease.
The researcher said efforts to enhance screening rates should be improved and more education on colorectal cancer is needed.
“That is where change starts, in my opinion,” Hassan said. “Start early, and I'm sure they would pass it on as they progress in life. Our findings will help raise awareness about this significantly persistent healthcare disparity. It may perhaps also act as a framework for evolution of colon cancer screening guidelines to incorporate modifiable risk factors.”
Hassan also said more study is needed to better understand the impact of COVID-19 pandemic and the reasons why the disease is so much deadlier in certain regions of the state and among minority populations.
Who is generally at risk for colorectal cancer?
As the name suggests, colorectal cancer is a cancer of the colon and rectum and tends to occur after age 40. However, recent studies have also shown increasing incidence in populations below the age of 40.
Patients with inflammatory bowel disease are also more at risk for developing the cancer, Hassan said. It’s important for those patients to be screened every eight to 10 years for signs of the disease.
Having a first-degree relative who has had colorectal cancer can also predispose someone to developing polyps — pre-cancerous lesions that can lead to the development of colorectal cancer, Hassan said.
Age, lifestyle factors, like smoking, sedentary living, obesity, a diet rich in red meat, salt and saturated fats or a low fiber diet can also make someone more predisposed to colorectal cancer.
Credits
Words: Rick Childress (UK Public Relations and Strategic Communication)
Graphic provided by Syed Hassan, M.D.

