2021 News Archive
July 2021
Featured Research & News
Cardiomyocyte Deletion of Bmal1 Exacerbates QT- and RR-Interval Prolongation in Scn5a +/ΔKPQ Mice
Schroder EA, Wayland JL, Samuels KM, Shah SF, Burgess DE, Seward T, Elayi CS, Esser KA, Delisle BP. Cardiomyocyte Deletion of Bmal1 Exacerbates QT- and RR-Interval Prolongation in Scn5a +/ΔKPQ Mice. Front Physiol. 2021 Jun 24;12:681011. doi:10.3389/fphys.2021.681011.
Circadian rhythms are generated by cell autonomous circadian clocks that perform a ubiquitous cellular time-keeping function and cell type-specific functions important for normal physiology. Studies show inducing the deletion of the core circadian clock transcription factor Bmal1 in adult mouse cardiomyocytes disrupts cardiac circadian clock function, cardiac ion channel expression, slows heart rate, and prolongs the QT-interval at slow heart rates.
What they did: This study determined how inducing the deletion of Bmal1 in adult cardiomyocytes impacted the in vivo electrophysiological phenotype of a knock-in mouse model for the arrhythmogenic long QT syndrome (Scn5a+/ΔKPQ). Electrocardiographic telemetry showed inducing the deletion of Bmal1 in the cardiomyocytes of mice with or without the ΔKPQ-Scn5a mutation increased the QT-interval at RR-intervals that were ≥130 ms.
What they found: Inducing the deletion of Bmal1 in the cardiomyocytes of mice with or without the ΔKPQ-Scn5a mutation also increased the day/night rhythm-adjusted mean in the RR-interval, but it did not change the period, phase or amplitude. Compared to mice without the ΔKPQ-Scn5a mutation, mice with the ΔKPQ-Scn5a mutation had reduced heart rate variability (HRV) during the peak of the day/night rhythm in the RR-interval. Inducing the deletion of Bmal1 in cardiomyocytes did not affect HRV in mice without the ΔKPQ-Scn5a mutation, but it did increase HRV in mice with the ΔKPQ-Scn5a mutation.
Why it matters: Deletion of Bmal1 in adult cardiomyocytes disrupts the expression profiles for a number of cardiac ion channel and transcription factor transcripts important for normal cardiac repolarization, depolarization, and conduction.
UK Experts Tackle Delta Variant Questions
As the SARS-CoV-2 delta variant continues to spread across the United States and hospitals’ COVID-positive intake numbers climb again, many questions remain around both vaccine effectiveness and vaccination rates, and what these numbers could mean moving into the fall.
Recently, a small panel of experts across the University of Kentucky and UK HealthCare participated in a discussion on these issues and what they mean for Kentucky. Becky Dutch , Ph.D., a virologist and the vice dean for research with the UK College of Medicine; Vince Venditto, Ph.D., an assistant professor of pharmaceutical sciences in the UK College of Pharmacy; Dr. Ashley Montgomery-Yates, UK HealthCare chief medical officer for inpatient and emergency services; and Dr. Aaron Grubbs, an infectious disease physician and UK HealthCare assistant medical director of infection prevention and control, are among the experts across various specialties at UK who are closely following the latest data trends.
So far, Venditto, who has extensive background in vaccine design and immunology, said that while evidence is evolving with regard to the delta variant, the COVID vaccines are doing what they are supposed to do against it so far.
“The vast majority of the people who are going to the hospitals right now with COVID infections are not vaccinated,” he said. “This is evidence that the vaccines are working. They are inducing the appropriate immune response to keep us protected, keep us out of the hospital and prevent death.”
Read the rest of the research story here.
Planning Implementation Success of Syncope Clinical Practice Guidelines in the Emergency Department Using CFIR Framework
Li J, Smyth SS, Clouser JM, McMullen CA, Gupta V, Williams MV. Medicina (Kaunas). 2021 Jun 3;57(6):570. doi: 10.3390/medicina57060570.
https://pubmed.ncbi.nlm.nih.gov/34204986/.
Overuse and inappropriate use of testing and hospital admission are common in syncope evaluation and management. Though guidelines are available to optimize syncope care, research indicates that current clinical guidelines have not significantly impacted resource utilization surrounding emergency department (ED) evaluation of syncope. Matching implementation strategies to barriers and facilitators and tailoring strategies to local context hold significant promise for a successful implementation of clinical practice guidelines (CPG). Our team applied implementation science principles to develop a stakeholder-based implementation strategy.
What they did: We partnered with patients, family caregivers, frontline clinicians and staff, and health system administrators at four health systems to conduct quantitative surveys and qualitative interviews for context assessment. The identification of implementation strategies was done by applying the CFIR-ERIC Implementation Strategy Matching Tool and soliciting stakeholders' inputs. We then co-designed with patients and frontline teams, and developed and tested specific strategies.
What they found: A total of 114 clinicians completed surveys and 32 clinicians and stakeholders participated in interviews. Results from the surveys and interviews indicated low awareness of syncope guidelines, communication challenges with patients, lack of CPG protocol integration into ED workflows, and organizational process to change as major barriers to CPG implementation. Thirty-one patients and their family caregivers participated in interviews and expressed their expectations: clarity regarding their diagnosis, context surrounding care plan and diagnostic testing, and a desire to feel cared about. Identifying change methods to address the clinician barriers and patients and family caregivers' expectations informed development of the multilevel, multicomponent implementation strategy, MISSION, which includes patient educational materials, mentored implementation, academic detailing, Syncope Optimal Care Pathway and a corresponding mobile app, and Lean quality improvement methods. The pilot of MISSION demonstrated feasibility, acceptability and initial success on appropriate testing.
Why it matters: Effective multifaceted implementation strategies that target individuals, teams, and healthcare systems can be employed to plan successful implementation and promote adherence to syncope CPGs.
Time-Restricted Eating May Reduce Diabetes-Related Hypertension
A new University of Kentucky College of Medicine study suggests that time-restricted eating may be able to help people with Type 2 diabetes reduce nocturnal hypertension, which is characterized by elevated blood pressure at night.
The study published in PNAS June 22 found that time-restricted eating, a routine in which eating is restricted to a specific window of time during each day, helped prevent and improve diabetes-related nocturnal hypertension in mice.
Study authors Ming Gong, Ph.D., M.D., professor in the Department of Physiology, and Zhenheng Guo, Ph.D., professor in the Department of Pharmacology and Nutritional Sciences, are hopeful their findings will mean time-restricted eating could offer similar benefits for people.
“We are excited about these findings and the implications they could have in future clinical studies," said Guo. “In addition to lifestyle changes like diet and exercise, time-restricted eating could have a healthy impact on people with Type 2 diabetes.”
Read the rest of the UKNOW story here.
When COVID-19 Took His Breath, a Double Lung Transplant Gave It Back
It seemed like nothing at first. Dave Hoover thought he had a sinus infection.
“I had a lot of pressure behind my eyes and in my sinus cavities,” he said. “I started feeling worse on my way home from work and stopped by the immediate care clinic to be seen. They tested me for COVID.”
The test was positive.
That was Jan. 26, 2021. A week later, Dave’s health took a drastic turn for the worse and he was admitted to his local hospital with bilateral COVID pneumonia.
Dave was, by all metrics, in perfect health. As an amateur bodybuilder, he worked out five days a week and followed a strict diet. After his son was born, he eased off from the gym, but still got plenty of exercise clearing the land on the farm he and his wife Emily bought in Stanford. They had just finished building their house and were looking forward to working the land in nicer weather when Dave got sick.
But after weeks in the hospital, his health continued to decline.
Read the rest of the UKNow story to learn how the ECMO team, Drs Baz, Keshavamurthy, Dwarakanath and Malyala successfully completed one of the few double lung transplants in the country.
June 2021
Featured Research and News
5th generation vs 4th generation troponin T in predicting major adverse cardiovascular events
Gupta V, Paranzino M, Alnabelsi T, Ayoub K, Eason J, Mullis A, Kotter JR, Parks A, May L, Nerusu S, Dai C, Cleland D, Leung SW, Sorrell VL. 5th generation vs 4th generation troponin T in predicting major adverse cardiovascular events and all-cause mortality in patients hospitalized for non-cardiac indications: A cohort study. PLoS One. 2021. 9;16(2):e0246332. doi: 10.1371/journal.pone.0246332.
https://pubmed.ncbi.nlm.nih.gov/33561174/
The frequency and implications of an elevated cardiac troponin (4th or 5th generation TnT) in patients outside of the emergency department or presenting with non-cardiac conditions is unclear.
What they did: Consecutive patients aged 18 years or older admitted for a primary non-cardiac condition who had the 4th generation TnT drawn had the 5th generation TnT run on the residual blood sample. Primary and secondary outcomes were all-cause mortality (ACM) and major adverse cardiovascular events (MACE) respectively at 1 year.
What they found:918 patients were included (mean age 59.8 years, 55% male) in the cohort. 69% had elevated 5th generation TnT while 46% had elevated 4th generation TnT. 5th generation TnT was more sensitive and less specific than 4th generation TnT in predicting both ACM and MACE. The sensitivities for the 5th generation TnT assay were 85% for ACM and 90% for MACE rates, compared to 65% and 70% respectively for the 4th generation assay. 5th generation TnT positive patients that were missed by 4th generation TnT had a higher risk of ACM (27.5%) than patients with both assays negative (27.5% vs 11.1%, p<0.001), but lower than patients who had both assay positive (42.1%). MACE rates were not better stratified using the 5th generation TnT assay.
Why it matters: In patients admitted for a non-cardiac condition, 5th generation TnT is more sensitive although less specific in predicting MACE and ACM. 5th generation TnT identifies an intermediate risk group for ACM previously missed with the 4th generation assay.
UK Research on Beige Fat Formation for Improved Glucose Metabolism Highlighted by NIDDK
Research led by University of Kentucky endocrinologist and Center for Clinical & Translational Science director Dr. Philip Kern was recently highlighted by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) in its 2021 Recent Advances & Emerging Opportunities report. The publication conveys important accomplishments resulting from NIDDK-funded research, as well as the enormous promise this research holds for the future. A multidisciplinary team from across UK’s campus contributed to the research.
This research demonstrated for the first time that a medication called mirabegron, already FDA-approved to treat overactive bladder, improves multiple measures of glucose metabolism in people who are overweight/obese with insulin resistance by inducing beige fat formation in their white adipose fat tissue. The findings uncover a potential new mechanism for treatment of diabetes. See the rest of the UKNOW Story here.
Funding for this research was provided by National Institutes of Health grant R01DK112282. The UK Center for Clinical and Translational Science is funded by NIH grant UL1TR001998.
TISA Alliance Podcast Series
The next installment in our TISA mentor reflections podcast series features Jeffery Talbert, PhD, professor and division chief for Biomedical Informatics in the UK College of Medicine and Professor in the Department of Pharmacy Practice and Science in the College of Pharmacy.
Click here to listen to the podcast. You will need to log in with your LinkBlue ID.
Alliance Research Initiative Provides 'Great Opportunity' for Graduate Student
Hammodah Alfar is in his second year of graduate school in the UK College of Medicine Department of Molecular and Cellular Biochemistry, with a specialized interest in platelet biology.
He has gained important research experience as a member of the Virus-Induced Thrombosis Alliance (VITAL), led by Beth Garvy, PhD, associate dean for biomedical education, and Sidney Whiteheart, PhD, professor of molecular and cellular biochemistry.
The VITAL Alliance investigates how viral diseases increase the risk of blood clotting, which is exactly what Alfar wanted to study for his PhD project. So far through the Alliance, he has helped collect samples and has gained valuable knowledge from studying them.
See the rest of the In the Loop Story here.
Associations of muscle lipid content with physical function and resistance training outcomes in older adults: altered responses with metformin
Long DE, Peck BD, Tuggle SC, Villasante Tezanos AG, Windham ST, Bamman MM, Kern PA, Peterson CA, Walton RG. Associations of muscle lipid content with physical function and resistance training outcomes in older adults: altered responses with metformin. Geroscience. 2021 Apr;43(2):629-644. doi: 10.1007/s11357-020-00315-9.
https://pubmed.ncbi.nlm.nih.gov/33462708/
Preserving muscle mass and strength is critical for long-term health and longevity. Age-related muscle lipid accumulation has been shown to be detrimental to muscle health
What they did: In healthy older individuals, we sought to determine whether muscle lipid content, determined from computed tomography, is associated with self-reported physical function, laboratory-measured performance, and the response to progressive resistance training (PRT), and how metformin may alter these responses.
What they found: For the first time, we show that metformin use during PRT blunted density and strength gains by inhibiting fiber type switching primarily in those with low baseline thigh muscle density. These results indicate that participants with higher muscle lipid content derive the most performance benefit from PRT.
Why it matters: Our results further indicate that muscle density may be as influential as muscle size for strength, physical function, and performance in healthy older adults.
VITAL: An Alliance Building the Infrastructure to Expand UK’s Disease Research Capability
Beth Garvy, PhD, and Sidney Whiteheart, PhD, originally planned to study blood clotting in HIV-positive patients when they first approached one another to establish a unified research team. Then COVID-19 emerged, and their focus shifted on the disease that started a global pandemic.
Dr. Garvy and Dr. Whiteheart now lead what is called the Virus-Induced Thrombosis Alliance (VITAL), a team supported by the University of Kentucky College of Medicine’s Alliance Research Initiative that is working to bridge the gap between infectious diseases and cardiovascular diseases, one of the Research Priority Areas from the UK Office of the Vice President for Research. Dr. Garvy is associate dean for biomedical education and professor in the department of microbiology, immunology, and molecular genetics, while Dr. Whiteheart is a professor of molecular and cellular biochemistry.
The short game of VITAL is to generate publications and collaborate on grants that fund critical research projects. The long game is a much greater goal – establishing a research infrastructure that will make studying infectious diseases a much smoother, more efficient process for clinicians and scientists so when new viruses inevitably appear, as COVID-19 did, UK will be even more prepared for tackling related issues.
Read the rest of the In The Loop story here. You will need to log in with your UK LinkBlue ID.
Convocation Award Winners
Academic Convocation is an annual presentation of awards to students and faculty for outstanding achievement in academics, service, research and teaching. Due to the pandemic, our 2019-2020 Academic Convocation Awards were postponed, and we are excited to finally announce our recipients.
CV-RPA Faculty Award Winners of the 2019-2020 Academy of Medical Education Excellence in Medical Education Awards were:
Vedant Gupta, MD
Department of Internal Medicine
Sibu Saha, MD
Department of Surgery
May 2021
Featured Research and News
Intracranial VCAM1 at time of mechanical thrombectomy predicts ischemic stroke severity
Maglinger B, Sands M, Frank JA, McLouth CJ, Trout AL, Roberts JM, Grupke S, Turchan-Cholewo J, Stowe AM, Fraser JF, Pennypacker KR. Intracranial VCAM1 at time of mechanical thrombectomy predicts ischemic stroke severity. J Neuroinflammation. 2021 May 11;18(1):109. doi: 10.1186/s12974-021-02157-4.
https://pubmed.ncbi.nlm.nih.gov/33971895/
Emergent large vessel occlusion (ELVO) strokes are devastating ischemic vascular events for which novel treatment options are needed. Using vascular cell adhesion molecule 1 (VCAM1) as a prototype, the objective of this study was to identify proteomic biomarkers and network signaling functions that are potential therapeutic targets for adjuvant treatment for mechanical thrombectomy.
What they did: The blood and clot thrombectomy and collaboration (BACTRAC) study is a continually enrolling tissue bank and registry from stroke patients undergoing mechanical thrombectomy. Plasma proteins from intracranial (distal to clot) and systemic arterial blood (carotid) were analyzed by Olink Proteomics.
What they found:VCAM1 levels indicating elevated levels of systemic and intracranial VCAM1 are associated with reduced improvement of stroke severity based on NIHSS from admittance to discharge. STRING-generated analyses identified biologic functional descriptions as well as function-associated proteins from the predictive models of infarct and edema volume.
Why it matters: The current study provides novel data on systemic and intracranial VCAM1 in relation to stroke comorbidities, stroke severity, functional outcomes, and the role VCAM1 plays in complex protein-protein signaling pathways. These data will allow future studies to develop predictive biomarkers and proteomic targets for drug development to improve our ability to treat a devastating pathology.
COVID-19 and Heart Transplant: A Case Series and Review of the Literature
Ballout JA, Ahmed T, Kolodziej AR. COVID-19 and Heart Transplant: A Case Series and Review of the Literature. Transplant Proc. 2021 Feb 25:S0041-1345(21)00137-8. doi: 10.1016/j.transproceed.2021.02.015. https://pubmed.ncbi.nlm.nih.gov/33795149/
Coronavirus disease 2019 (COVID-19) has resulted in many challenges in patient care, especially among high-risk populations such as heart transplant recipients. Patients with heart transplant experience a significantly higher mortality rate with COVID-19 infection, and management is based on extrapolation from clinical trials done on nontransplant patients and from clinical experience.
What they did: Here we report 4 cases of patients with heart transplant who presented with COVID-19 infection in late 2020. Patients presented with symptoms similar to those seen in the general population. All 4 patients were admitted to the hospital, and they were all treated with dexamethasone. In addition, 2 patients received remdesivir.
What they found: Immunosuppressive medications were adjusted to maintain adequate levels of immunosuppression but at the same time allow for an adequate immune response against the infection. All patients were discharged alive from the hospital.
Why it matters: These cases and literature search allowed us to develop suggestions for a standardized care management approach in transplant patients with COVID-19.
May News
Transdisciplinary Implementation Science Alliance (TISA) Podcast Series
TISA Podcast
The TISA alliance shared their first installment in the TISA mentor reflections podcast series, a series of conversations with senior clinician researchers and implementation scientists where they share advice and lessons learned about career development. Our first interview is with Susan Smyth, MD, PhD, FACC, director of Gill Heart and Cardiovascular Institute, chair of the Division of Cardiovascular Medicine and a successful physician researcher. Dr. Smyth is interviewed by Gretchen Wells, MD, PhD, Professor and Director of the Women's Heart Health program.
The audio of the interview is attached, click on the image about to listen. You will need to log in with your LinkBlue ID. If you would like copies of the podcast series, please email cmcmu2@uky.edu.
UK Professor Awarded $1.9M for Sepsis Research
Xiangan Li, a professor in the Department of Physiology and the Saha Cardiovascular Research Center, received the prestigious R35 grant from the NIH’s National Institute of General Medical Sciences (NIGMS), which will fund sepsis research in his lab over the next five years.
Sepsis is a life-threatening condition that occurs when an infection triggers a chain reaction throughout the body. Without timely treatment, it can quickly lead to tissue damage, organ failure and death. The Centers for Disease Control and Prevention reports that nearly 270,000 Americans die as a result of sepsis every year, and one in three patients who die in a hospital has sepsis.
Li studies how hormones called glucocorticoids regulate the body’s immune system in response to sepsis. Glucocorticoids are released by the adrenal glands and help to reduce certain aspects of immune function such as inflammation. They are often supplemented as a therapy to treat sepsis and other diseases caused by an overactive immune system. However, not all sepsis patients may benefit from additional glucocorticoids, Li says.
See the rest of the story here: https://research.med.uky.edu/news/uk-professor-awarded-19m-sepsis-research
MYRA: An Alliance Finding Innovative Approaches for Improved Cardiac Recovery
For many years, ventricular assist devices (VADs) were considered a last resort for patients with serious heart failure. These mechanical pumps, which help maintain blood circulation, were mainly used for patients awaiting a heart transplant.
Recent studies conducted by University of Kentucky researchers suggest VADs actually could be used to recover the hearts of patients with heart failure, even those with advanced heart failure, possibly preventing their need for transplants in the future.
Holding this research at UK could be groundbreaking for the state of Kentucky. UK HealthCare performs more than 40 heart transplants per year, or one percent of heart transplants worldwide.
Emma Birks, MD, PhD, and Ken Campbell, PhD, are co-principal investigators of the Myocardial Recovery Alliance (MYRA), a team established under the UK College of Medicine’s Alliance Research Initiative. Together, with a team of highly qualified cardiovascular experts and scientists across campus, they’re leading revolutionary studies that could change standards of cardiac care in real time.
Read the rest of the story here. To learn more about UK-AARC and other Alliance teams, visit Aortopathy Alliance Research Center (UK-AARC).
CCTS Research Day on Demand
CCTS Research Days content is now available ON DEMAND for those who previously registered AND to those who still wish to register. Viewers can still give anonymous feedback on posters using the general feedback link.
https://www.labroots.com/virtual-event/ccts-spring-research-day-2021
Alliance "Visiting" Speaker Series
TISA Virtual Presenter Event: Anne Sales, PhD, RN
University of Michigan
Date: Jun 21, 2021 - 2:00pm to 3:30pm
Register to attend and receive a calendar invite: https://uky.zoom.us/j/82069349232?pwd=eCt0ZzkwQXpHS1U3Ti80aVlsUER3Zz09
April 2021
Featured Research
The Prorenin Receptor and its Soluble Form Contribute to Lipid Homeostasis
Eva Gatineau, Gertrude Arthur, Audrey Poupeau, Kellea Nichols, Brett T. Spear, Nathan R. Shelman, Gregory Graf, Ryan Temel, Frédérique Yiannikouris. Am J Physiol Endocrinol Metab. 2021 Mar 1;320(3):E609-E618. doi:10.1152/ajpendo.00135.2020. https://pubmed.ncbi.nlm.nih.gov/33459178/
Obesity is associated with several deleterious changes in lipid metabolism and alterations in hepatic lipid metabolism. Hyperlipidemia is a risk factor for cardiovascular disease and is estimated to be responsible for more than half of cardiovascular mortality. We previously identified the prorenin receptor (PRR) as a potential contributor to liver steatosis.
What they did: In this study, we investigated the contribution of PRR and its soluble form, sPRR, to lipid homeostasis. PRR-floxed male mice were treated with an adeno-associated virus with thyroxine-binding globulin promoter driven Cre to delete PRR in the liver (Liver PRR KO mice).
What they found: The deletion of PRR in liver induced hepatomegaly, hypercholesterolemia, liver inflammation and injury, and disrupted hepatic lipid homeostasis causing an increase in hepatic cholesterol and a decrease in hepatic triglycerides contents. In addition, the deletion of hepatic PRR lowered hepatic LDLR and SORT1 proteins but stimulated hepatic cholesterol synthesis (up-regulation of hepatic SREBP2 and HMG CoA-R genes) suggesting that hepatocyte sensed a shortage in cholesterol uptake and, to compensate, increased cholesterol synthesis. The measurement of total sPRR contents in fat indicated that the increase in circulating sPRR, observed in Liver PRR KO mice, originated from the adipose tissue. Mechanistic studies performed in vitro indicated that PRR contributed to triglycerides homeostasis through a PRR-PPARγ dependent mechanism whereas both PRR and sPRR contributed to hepatic cholesterol homeostasis.
Why it matters: The remarkable phenotype demonstrated the importance of liver PRR and sPRR in lipid homeostasis and highlighted a new paradigm of crosstalk between the liver and the adipose tissue.
Extracorporeal Life Support and Mechanical Circulatory Support in Out-of-Hospital Cardiac Arrest and Refractory Cardiogenic Shock
Gunn TM, Malyala RSR, Gurley JC, Keshavamurthy S. Interv Cardiol Clin. 2021 Apr;10(2):195-205. doi: 10.1016/j.iccl.2020.12.006.
https://pubmed.ncbi.nlm.nih.gov/33745669/
Highlights of this manuscript:
• The prevalence of extracorporeal cardiopulmonary resuscitation is increasing worldwide as more health care centers develop the necessary infrastructure, protocols, and technical expertise.
• Early initiation of venoarterial (VA) extracorporeal life support (ECLS) in cases of refractory cardiogenic shock has been shown to improve survival and neurologic outcomes.
• Left ventricle unloading is an essential component of VA ECLS in the setting of cardiogenic shock and associated left ventricular dilation and is associated with improved survival and favorable outcomes.
April 2021 Award Winners
Cardiovascular Research Priority Area DREAM Scholar
Since 2018, the Disparities Researchers Equalizing Access for Minorities (DREAM) Scholars Program has supported the training of exceptional, underrepresented pre-docs, post-docs and assistant professors at the University of Kentucky who are committed to health equity research.
The program originally began in 2015 as mentoring program in the UK College of Nursing for “people who needed to belong—racial, sexual, and gender minorities”, said Lovoria Williams, Ph.D., who currently co-directs DREAM. Now led by the Center for Clinial and Translational Science (CCTS) and the Center for Health Equity Transformation (CHET), DREAM has evolved into a robust, multidisciplinary career development opportunity for researchers from across UK’s colleges.
Most recently, the impact and importance of the program compelled the UK Markey Cancer Center and the Cardiovascular Research Priority Area to each sponsor an additional DREAM Scholar position per year, bringing the total number from five to seven.
Firaz Peer, Ph.D. (Scholar)
Assistant Professor, College of Communication and Information
Research Topic: Exploring religio-cultural interventions in substance abuse treatment information infrastructures
Mentor: Hilary Surrat, Ph.D.
See the rest of the DREAM Schollars and more information about the program here.
April 2021 News
Physiology Professor Appointed to Journal’s Editorial Leadership Team
The Journal of Lipid Research, a peer-reviewed journal published by the American Society for Biochemistry and Molecular Biology, has appointed six junior faculty members to its editorial leadership team. One of the appointments is Scott M. Gordon, assistant professor in the Department of Physiology at the University of Kentucky College of Medicine, where his lab studies intestinal lipid absorption and atherosclerotic cardiovascular disease.
UK-AARC: An Alliance Reflecting the Strength of UK’s Aortic Research
Twenty years ago, University of Kentucky researchers Alan Daugherty, PhD, DSc, and Lisa Cassis, PhD, stumbled into a research method that contributed greatly to UK’s cardiovascular research growth.
Together, they found a way to develop aortic diseases using an animal model that has now become a widely used approach to study aortic disease. This aortic disease model has been used not only to understand how the disease forms, but also as an avenue to study promising new therapies. As a result, the impact of their cardiovascular research grew and attracted high-level faculty to UK. Their group expanded, establishing a framework for the unified team they lead today.
Dr. Daugherty, professor and chair of physiology and director of the Saha Cardiovascular Research Center, and Dr. Cassis, professor of pharmacology and nutritional sciences and UK Vice President for Research, are co-principal investigators of the Aortopathy Alliance Research Center (UK-AARC). Under the College of Medicine’s Alliance Research Initiative, UK-AARC is a structured team of researchers and clinicians bringing a wide range of expertise to better understand diseases of the aorta, the body’s largest artery.
Read the rest of the story here. To learn more about UK-AARC and other Alliance teams, visit www.med.uky.edu/alliance.
ASE Announces New Editor-in-Chief of CASE, the Premier Cardiovascular Imaging Case Reports Journal
April 14, 2021, Durham, NC – The American Society of Echocardiography (ASE) is proud to announce that Vincent L. Sorrell, MD, FACC, FASE, FSCCT, FSCMR, has accepted the position of CASE Editor-in-Chief (EIC) starting August 1, 2021. CASE, ASE’s online, cardiovascular imaging case reports journal, publishes case reports where cardiovascular ultrasound is used to help diagnose or solve a clinical problem in humans or animals. This popular open access educational platform features cases where cardiovascular ultrasound was used as a critical component of a multimodality approach to disease diagnosis or evaluation or where it was used to detect unusual or atypical disease manifestations.
The current Editors-in-Chief, Karen G. Zimmerman, BS, ACS, RDCS, RVT, FASE, and L. Leonardo Rodriguez, MD, FASE, FACC, who founded this thriving publication five years ago, are thrilled with the choice of Dr. Sorrell. ASE President Judy Hung, MD, FASE, said, “ASE is so fortunate to have been able to select Vince to be Editor-in-Chief of CASE. The excellence and enthusiasm that Vince will bring to this position is very exciting, and Vince will be a driving force for CASE’s quality of content and growth.”
Dr. Sorrell is the Anthony N. DeMaria Professor of Medicine, Interim Chair of the Division of Cardiovascular Medicine, and Program Director of the Adult Cardiovascular Fellowship at the University of Kentucky, Gill Heart and Vascular Institute in Lexington, Kentucky. He is a member of the ASE Board of Directors, was awarded the 10th annual Richard Popp Excellence in Teaching Award in 2010, was elected to the Association of University Cardiologists in 2019, and also serves as an Associate Editor for the Journal of the American Society of Echocardiography (JASE). Dr. Sorrell is the author of over 127 research articles, and numerous book chapters, and has been involved in several textbooks. Under Dr. Sorrell’s direction, CASE will transition from a bi-monthly publication to monthly starting in January 2022.
Dr. Sorrell said, “I am extremely excited to serve as the EIC of this phenomenal cardiovascular imaging case journal. I believe that digital media provides opportunities for education previously unattainable and that case-based education remains critical in today’s rapidly changing environment dominated by visual learners. Working closely with the dedicated CASE Editorial Team of imaging experts from around the world, we hope to provide readers with many novel avenues aimed at linking imaging findings to clinical outcomes. Keep your eye out for our new CASE/JASE Spotlights, Guideline Highlights, Author Interviews, Puzzles, Annual ShowCASE events, and more. If you have ideas for case-based learning techniques or would like to contribute in any way to the success of CASE, please reach me at @CASEfromASE, @VLSorrellImages, or at CASE4ASE@gmail.com.”
Saha Legacy Continues with Establishment of New Research Center
A new research center focused on aortic disease has been established at the University of Kentucky thanks to a gift from the Saha Foundation.
Housed in the Biomedical Biological Science Research Building on the UK campus, the Saha Aortic Center will promote research and education to advance clinical care for disease of the aorta. Aortic disease can cause the expansion and rupture of a vessel wall in the chest or abdominal area, leading to potentially deadly internal bleeding.
Alan Daugherty, Ph.D., chair of the Department of Physiology and director of the Saha Cardiovascular Research Center in the UK College of Medicine, will serve as director of the Saha Aortic Center.
“Aortic disease affects the major artery that carries blood from the heart to the rest of the body,” Daugherty said. “Having this center that specifically focuses on research and education in this field is vital.”
David Minion, MD, program director and professor of Vascular Surgery, and Mary Sheppard, MD, assistant professor of Family and Community Medicine, Surgery and Physiology, will serve as co-directors for the center.
“Dr. Saha has devoted a lifetime of service to the health care needs of Kentucky. The generous gift attests to his and his family’s passion and dedication to our Commonwealth,” Minion said. “I am honored to be a part of this exciting initiative.”
Se the rest of the UKNow story here.
500 Heart Transplants!
We performed our first heart transplant in 1991. Since that time, we’ve continued to care for those with end-stage heart failure by offering this life-saving procedure.
A week ago, we performed our 500th heart transplant. Thank you to each of our team members at UK and the UK Gill Heart & Vascular Institute who have been able to help provide a second chance at life. And most of all, thank you to those who donated, providing a gift of life.
Follow GHVI on Facebook https://www.facebook.com/GillHeartInstitute to see more GHVI happenings.
Join us for the Inaugural UK Implementation Science Research Day!
The first Implementation Science Research Day, part of CCTS Spring Research Day, will be held virtually April 7 and 8, 2021! Please submit abstracts for oral presentations or for posters with an Implementation Science theme here.
March 2021
Featured Research
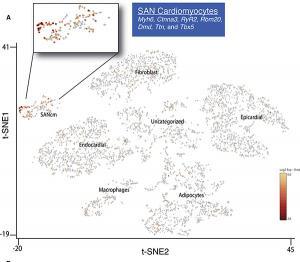
Rad-GTPase contributes to heart rate via L-type calcium channel regulation
Levitan BM, Ahern BM, Aloysius A, Brown L, Wen Y, Andres DA, Satin J. J Mol Cell Cardiol. 2021 Feb 6;154:60-69. doi: 10.1016/j.yjmcc.2021.01.005.
Highlights of this manuscript:
• Sinoatrial node (SAN) cardiomyocytes express Rad.
• Rad deletion in SAN cardiomyocytes increases I Ca,L. This is consistent with Rad's role as an endogenous L-type calcium channel (LTCC) governor.
• Rad regulates intrinsic heart rate (HR) consistent with βAR modulated I Ca,L regulation.
• HR during the sleep cycle is selectively elevated by Rad deletion.
• Diurnal variation of HR is preserved, albeit with reduced amplitude.
• Rad – LTCC association may be a useful target for future therapeutics to treat symptomatic bradycardia.
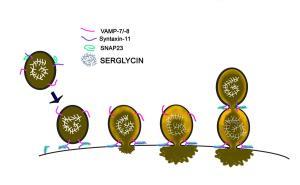
Platelet α-Granule Cargo Packaging and Release are Affected by the Luminal Proteoglycan, Serglycin
Chanzu H, Lykins J, Wigna-Kumar S, Joshi S, Pokrovskaya I, Storrie B, Pejler G, Wood JP, Whiteheart SW. J Thromb Haemost. 2021 Jan 15. https://pubmed.ncbi.nlm.nih.gov/33448622/
Upon injury to a blood vessel, platelets activate and secrete cargo stored in three classes of membrane-bound granules, dense, α, and lysosomes. Secretion is vital for normal clotting, and excessive release can promote occlusive thrombosis. This manuscript examined how an intragranular proteoglycan, serglycin (SRGN), affects the packaging of α-granule cargo and their release once granule plasma membrane fusion has occurred. SRGN is an 18 kDa core protein decorated with up to eight glycosaminoglycans (GAGs) chains attached to serine residues. The size, type, and levels of the attached glycans depend on the species and the cell type. Chondroitin sulfate (CS) and dermatan sulfate (DS) decorate the core SRGN protein in platelets. Previously reported, platelets lacking SRGN showed defective aggregation and thrombus formation.
What they did and what they found: To understand how SRGN affects platelet granule packaging, cargo release, and extra-platelet microenvironments, we examined platelets from SRGN-/- and SRGN+/+ control mice. Metabolic, 35SO4 labeling showed that SRGN was a major sulfated macromolecule in megakaryocytes. SRGN colocalized with α-granule markers [Platelet Factor 4 (PF4), von Willebrand Factor (vWF), and P-Selectin], but its deletion did not affect α-granule morphology or number. However, granule composition was altered. Some α-granule proteins, e.g., P-Selectin, vWF, fibrinogen, were unaffected, but basic proteins (pI ≥ 8), e.g., PF4, SDF-1, Angiogenin, were significantly reduced. Markers for dense granules, serotonin (5-HT) and lysosomes, β-hexosaminidase (HEXB) were slightly elevated. Thrombin-induced exocytosis of PF4 was also greatly reduced while the release of RANTES/CCL5 was normal and osteopontin (OPN; pI 4.34) secretion was more rapid. The secretion of 5-HT, and HEXB were normal. Electron microscopy studies showed distinct morphologies in activated platelets. The α-granule lumen of SRGN-/- platelet had a grainy appearance, while that of wild-type granules had only fibrous material remaining. α-Granule swelling and decondensation were also reduced in SRGN-/- platelets suggesting that SRGN affects how granule cargo is dissolved for release. Upon stimulation of wild-type platelets, a SRGN/PF4 complex was released in a time- and agonist-dependent manner. Such complexes may affect the extra-platelet environment since shedding of surface GPVI was modestly enhanced in SRGN-/- platelets.
Why it matters: Our data show that SRGN influences α-granule packaging, cargo release, and shedding of platelet membrane proteins. This suggests that the physical chemistry of this polyanionic proteoglycan not only affect intragranular microenvironments but also extra-platelet ones.
Unique Surgical Approach for Heart Failure Patients
Kyle Groves is rooted in the farm. He took over his family’s fifth-generation dairy farm business in 1969.
“The day begins before the sun rises and ends after sunset,” Groves, of West Virginia, said. “My life revolved around the farm.”
Groves’ days continued this way for 23 years until one day in 1992, he suffered his first heart attack at 48 years old. It was just the beginning of a long road of heart problems to come. Over the years, Groves had six bypasses, an internal cardiac defibrillator (ICD) and cardiac resynchronization therapy (CRT) in 2015. Most recently, after feeling weak and unable to do the things he previously enjoyed, heart surgeons at UK HealthCare (UKHC) placed a left ventricular assist device (LVAD).
A VAD is a mechanical device that supports the heart by pumping blood through the body when the patient’s heart cannot perform properly. This can be a short-term placement while the patient awaits a heart transplant, or for long-term support in patients who cannot receive a heart transplant.
As a resident of Canvas, West Virginia, Groves receives care through the Congestive Heart Failure Clinic at Charleston Area Medical Center. His doctors referred him to UK HealthCare Gill Heart & Vascular Institute for advanced heart failure care. Dr. Emma Birks, heart failure cardiologist, and Dr. Rajasekhar Malyala, cardiovascular and thoracic surgeon and assistant professor of surgery, treated Groves before and during his LVAD surgery.
See the rest of the UKNow story here.
March 2021 News
Susan Smyth MD, PhD Named Dean of UAMS College of Medicine
Congratulations to Dr. Susan Smyth, who has been named executive vice chancellor and dean of the College of Medicine at the University of Arkansas for Medical Sciences (UAMS).
She begins this new role on June 1.
Dr. Smyth's work as a professor, clinician, and researcher has been vital to our institution, and we are grateful for her contributions, most recently as division chief of cardiovascular medicine and director of the UK Gill Heart and Vascular Institute.
Thank you, Dr. Smyth, for everything you've done to help further our mission and help improve Kentucky health!
Click Here to Read the Full Announcement from UAMS
February 2021
Featured Research
Donor-specific phenotypic variation in hiPSC cardiomyocyte-derived exosomes impacts endothelial cell function
https://pubmed.ncbi.nlm.nih.gov/33416449/
Turner A, Aggarwal P, Matter A, Olson B, Gu CC, Hunt SC, Lewis CE, Arnett DK, Lorier R, Broeckel U.Am J Physiol Heart Circ Physiol. 2021 Mar 1;320(3):H954-H968. doi: 10.1152/ajpheart.00463.2020.
Exosomes are an important mechanism of cell-cell interaction in the cardiovascular system, both in maintaining homeostasis and in stress response. Interindividual differences that alter content in exosomes may play a role in cardiovascular disease pathology.
What they did: In this study, we characterized exosomal content in phenotypically diverse human induced pluripotent stem cell-derived CMs (hiPSC-CMs). Cell lines were generated from six participants in the HyperGEN cohort: three with left ventricular hypertrophy (LVH) and three with normal left ventricular mass (LVM).
What they found: Sequence analysis of the intracellular and exosomal RNA populations showed distinct expression pattern differences between hiPSC-CM lines derived from individuals with LVH and those with normal LVM. Functional analysis of hiPSC-endothelial cells (hiPSC-ECs) treated with exosomes from both hiPSC-CM groups showed significant variation in response, including differences in tube formation, migration, and proliferation.
Why it matters: These findings provide novel insight into underlying mechanisms of hypertrophic cell signaling between different cell types. With a growing interest in stem cells and exosomes for cardiovascular therapeutic use, this also provides information important for regenerative medicine.
Force-dependent recruitment from myosin OFF-state increases end-systolic pressure-volume relationship in left ventricle
Mann CK, Lee LC, Campbell KS, Wenk JF. Biomech Model Mechanobiol. 2020 Dec;19(6):2683-2692. doi: 10.1007/s10237-020-01331-6.
What they did: This work embeds a physiologically motivated cell-contraction model into a 3D computational model of the heart to more accurately simulate the cardiac cycle. Specifically, this contraction model features length-dependent activation via force-dependent recruitment of myosin heads out of the super-relaxed state.
What they found: Simulations of vena cava occlusion with this 3D model show a steeper end-systolic pressure-volume relationship (ESPVR) when compared to the same model with the super-relaxed state omitted.
Why it matters: This suggests that a force-dependent mechanism, which is responsible for the recruitment of thick filaments at the cell-level, contributes to the Frank-Starling relationship at the organ level.
New Study to Provide 1st In-Depth Look at Hip Pain in Patients with Marfan Syndrome
Researchers at the University of Kentucky have received a $100,000 grant from The Marfan Foundation to assess how patients with Marfan syndrome develop hip pain. The study will be conducted by Mary Sheppard, an assistant professor of family medicine and surgery in the UK College of Medicine, and Michael Samaan, an assistant professor of biomechanics in the UK College of Education Department of Kinesiology and Health Promotion. Marfan syndrome is a genetic condition that impacts the body’s connective tissue. It most frequently affects the heart, blood vessels, eyes and bones. Diagnostic features can include a dilated aorta; dislocated lens; long arms, legs and fingers; a curved spine; a chest that sinks in or sticks out; flat feet; and an abnormally shaped hip joint, among others. The cardiovascular impacts of having Marfan syndrome can be significant, and have been the focus of the majority of prior research. The study at UK will be a first-look at the mechanisms involved in the onset of hip joint pain and cartilage degeneration in patients with Marfan syndrome. Nearly half of patients with Marfan syndrome self-report hip joint pain yet it is highly unrecognized by clinicians. Read the rest of the UKNow article here. If you would like to learn more about participating in this study, please call Dr. Mary Sheppard at 859-323-3280.
January 2021
Featured Research
-
Circadian disruption with constant light exposure exacerbates atherosclerosis in male ApolipoproteinE-deficient mice. Chalfant, JM, Howatt DA, Tannock, LR, Daugherty A, Pendergast JS. Sci Rep. 2020 Jun 18;10(1):9920. doi: 10.1038/s41598-020-66834-9.
Disruption of the circadian system caused by disordered exposure to light is pervasive in modern society and increases the risk of cardiovascular disease. The mechanisms by which this happens are largely unknown.
What they did: In this study, we determined the effects of light-induced circadian disruption on atherosclerosis in ApoE-/- mice. We induced severe disruption of circadian rhythms by exposing ApoE-/- mice to constant light for 12 weeks.
What they found: Constant light exposure exacerbated atherosclerosis in male, but not female, ApoE-/- mice. Male ApoE-/- mice exposed to constant light had increased serum cholesterol concentrations due to increased VLDL/LDL fractions.
Why it matters: Taken together, these data suggest that exacerbated dyslipidemia may mediate atherosclerotic lesion formation caused by constant light exposure. - Perceived Control Prevents Perception of Negative Changes in Life as a Result of Caring for a Patient With Heart Failure. Chung ML, Liljeroos M, Moser DK, Lennie TA. J Cardiovasc Nurs. 2020 Jun 12:10.1097/JCN.0000000000000717. Click here for NCBI link.
Family caregivers of patients with heart failure (HF) commonly experience emotional distress and caregiving burden. Despite their caregiving distress, caregivers may experience positive or negative changes in their life compared with before caregiving. Greater perceived control is associated with better health outcomes, but little is known about whether perceived control is related to caregivers' perceptions of positive or negative changes in life, independent of their distress and burden in providing care for patients with HF.
What they did: Primary caregivers of patients with HF (N = 140, 75% women) completed questionnaires about perceived positive or negative changes in life as a result of caregiving, perceived control, depressive symptoms, anxiety, and caregiving burden.
What they found: Compared with caregivers who reported positive changes in life (42%), caregivers who perceived negative changes in life (58%) had higher levels of depressive symptoms, anxiety, and caregiving burden.
Why it matters: Practical interventions designed to enhance perceived control are needed for family caregivers to prevent experiencing a negative perception of life changes due to caregiving responsibility for patients with HF.